Background: Genomic alterations are a hallmark of hematological malignancies and comprise small nucleotide variants, copy number alterations and structural variants (SV). SV lead to the co-localization of remote genomic material resulting in 2 different scenarios: 1. breakpoints are located within 2 genes leading to a chimeric fusion gene and a fusion transcript, 2. breakpoints are located outside of genes, frequently placing one nearby gene under the influence of the regulatory sequences of the partner, leading to a deregulated - usually increased - transcription.
Aim: The frequency of fusion transcripts was determined across hematological entities in order to 1) identify recurrent partner genes across entities, 2) evaluate the specificity of fusion transcripts and genes involved in fusions for distinct entities.
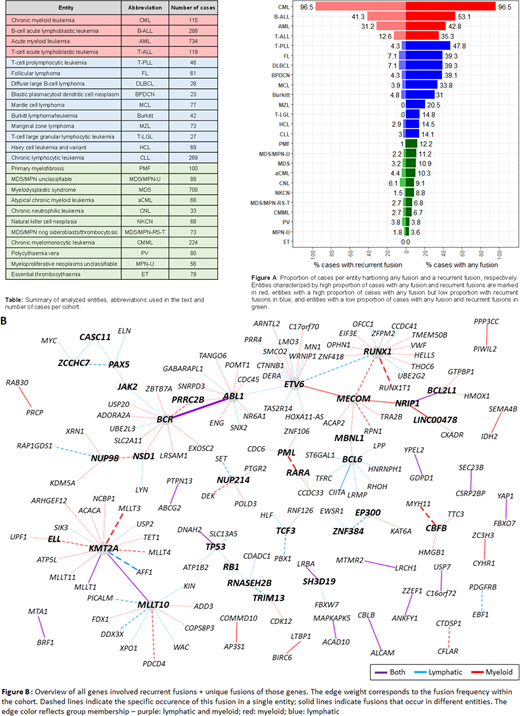
Cohort and Methods: Whole transcriptome sequencing (WTS) was performed in 3,549 patients in 25 different hematological entities (table). 101 bp paired-end reads were produced on a NovaSeq 6000 system (Illumina, San Diego, CA) with a yield between 35 and 125 million paired reads per sample. Potential fusions were called using 3 different callers (Arriba, STAR-Fusion, Manta), only fusions called by at least 2 callers, validated by whole genome sequencing (data available for all cases) and with at least one protein coding partner were kept for further analyses. Reciprocal fusion transcripts were counted as one fusion event.
Results: In total 1,309 fusion transcripts were identified in 932 of 3,549 (26.3%) patients. 221 patients showed > 1 fusion (2 fusions: 150, 3: 36, >3: 35). 806 distinct fusion transcripts were divided into recurrent fusions (n=50) and unique fusions, i.e. found only in 1 case (n=756).
Out of 932 patients with at least 1 fusion, 541 (58%) patients harbored a minimum of one recurrent fusion. The proportion of patients harboring any or a recurrent fusion varied substantially between different entities with high frequencies for both in CML (96.5%/96.5%), B-lineage ALL (53.1%/41.3%), AML (42.8%/31.2%), and T-lineage ALL (35.3%/12.6%). In several myeloid entities low fusion frequencies were observed (e.g. PMF, MDS/MPN-U, MDS, figure A). No fusion transcripts were detected in ET. Strikingly, fusions were detected in a substantial proportion of cases with lymphoid neoplasms but only very few occurred recurrently (e.g. T-PLL: 47.8%/4.3%, FL: 39.3%/4.9%, figure A). With regard to age, only patients with AML and T-ALL harboring recurrent fusions were significantly younger than corresponding cases without recurrent fusions (59 vs 71 yrs, p<0.0001; 35 vs 38 yrs, p=0.02). Only in AML patients with unique fusions were older (70 vs 66 yrs, p=0.02), while no age differences were observed between cases with and without unique fusions in other entities.
23/50 (46%) of the recurrent fusions were specific for one entity (12 in myeloid, 11 in lymphatic entities), while the other 54% (27/50) were observed in 2 to 7 different entities. Of these 27 recurrent fusions, only 16 fusions were shared between myeloid and lymphatic entities, while 10 were restricted to myeloid and one fusion to lymphatic entities (figure B). In total 1,270 different genes were involved in the 806 distinct fusions, indicating a broad spectrum of potential functional impact. 54 genes were involved only in recurrent fusions, 27 genes in both recurrent and unique fusions, while 1,189 genes were solely involved in unique fusions. Four genes involved in recurrent fusions and 32 genes involved in unique fusions are FDA approved drug targets (Human Protein Atlas).
Only 16% (199/1270) of the genes were involved in more than one fusion: 3 genes (ETV6, KMT2A, RUNX1) in 14 fusions, 2 genes (ABL1, BCR) in 11 fusions, 16 genes in 4 to 10 fusions, 38 genes in 3 fusions, 140 in 2 fusions. Several genes frequently involved in fusions in hematological malignancies (e.g. ABL1, ETV6, KMT2A) and 78/1189 genes only involved in unique fusions were also reported to be partners in fusions in non-hematological malignancies.
Conclusions: As known, in CML and acute several leukemias a high proportion of patients harbor fusions of which many occur recurrently, suggesting a substantial pathogenic impact and, thus, requiring detection in a diagnostic work-up. In BCR-ABL1 negative chronic myeloid malignancies few fusions were observed while lymphoma patients carry frequently non-recurrent fusions with so far unknown impact on pathogenesis and prognosis.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.